This is one of our most difficult moments. Please bear with me as time is a non existent concept for this event. However the fear and emotions of this night will live with us forever.
We had been in the NICU for a few weeks at this point. The girls had independent rooms but they were right next to each other. In fact they shared a wall with a window so I could be in either girls room and see the other so long as the shade was up. So for these first few weeks things were never easy, it feels like a slow progression forward and it can be frustrating being put on the fast track to learn and understand things around you. I was always present daily for rounds for each girl, to discuss their care plans. After that I spent most of my days going back and forth between each room to read, to talk, to help with each girls’ care and to hold them. However because both girls were so small and required so much help to get out I would hold a different girl everyday for hours at a time.
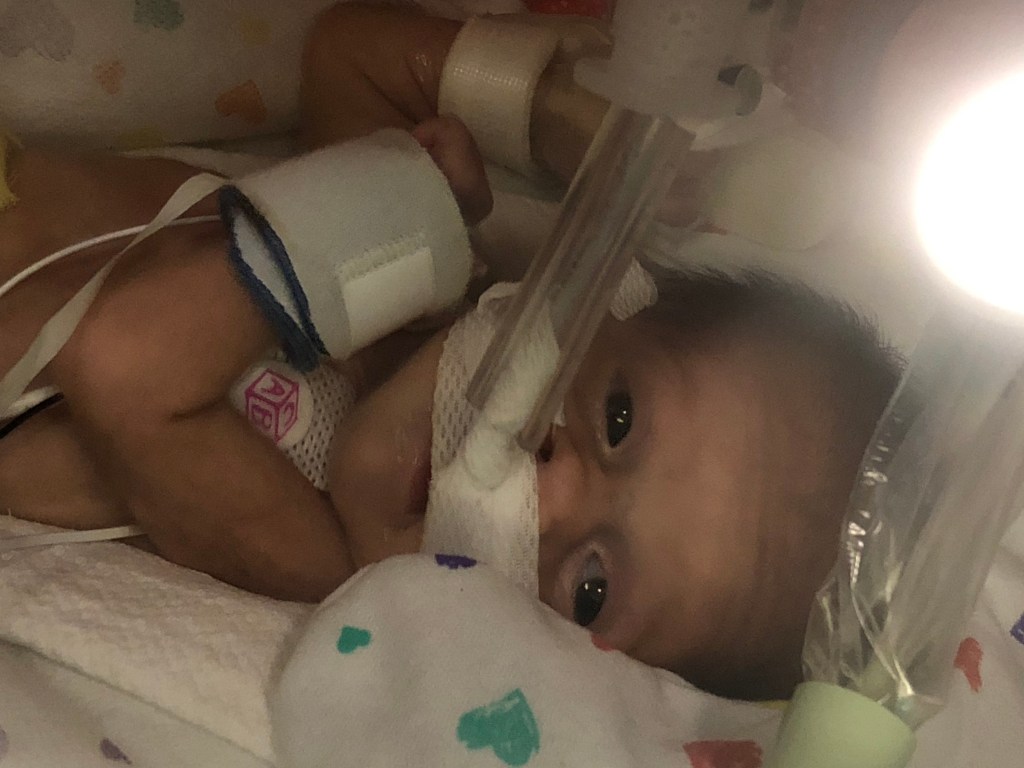
Matt was given the opportunity to get a light work schedule so he could be up as much as possible to see the girls. I remember it was a friday and he was coming up for the weekend. I spent that afternoon holding and snuggling and singing to Jocelyn. It was always a challenge to hold her and honestly very nerve wracking with all the tubes and wires she was dependent on to keep her alive. But I always tried to make the best out of every time I got to hold each girl. Matt wasn’t going to be able to get up to me early enough to hold Jocelyn consecutively to my holding time with her. Dinner was going to be served at Ronald Mcdonald at 6, so we decided to meet there first. Ronald Mcdonald provided me a close place to stay, shuttles to and from the hospital, and dinners provided every night to help families financially. After dinner then we would go back to visit the girls read them a story and say our good nights. I held Jocelyn until it was dinner time then had help to get her back into the incubator to head off. Once we finished eating we headed on back to CHOP. We walked into Jocelyn’s room first to meet her nurse who was already in there with her incubator lid up and start our night time routine. I put my bag down and walked over to the incubator. Matt was already over their asking what was wrong. That’s when I saw her, I’ll describe her color as grey however most medical staff term the color blue. Within seconds the code blue bell was called. “CODE BLUE, ROOM 80” I panicked as any mother would and immediately left the room and went to Lucy’s room in tears.This can’t be happening, why is this happening she was doing so well, she has to pull through. Jocelyn was in distress and flatlining.. I could see Jocelyn’s stats on Lucy’s monitor. My very first assumption was that it was her heart and I knew as well as anyone else in this room she was far too small to be able to save her if that was the case. I remember a flood of people running over to her room, and could see them through the window. We watched nervously as the tidal waves of doctors and nurses began utilizing any and everything possible from the crash cart. I remember the countless times she would stabilize for a minute then flat line again. Matt came into Lucy’s room minutes after and we both were in tears, hysterical tears. Praying, hoping this wasn’t it for her. Any medical staff member that came in to update us didnt know why or what was happening. Several nurses who didn’t know us or the girls would try to come in and take Jocelyn’s stats off of Lucy’s monitor. By the last one Matt and me snapped and told them not to touch it and that it was our daughter, we needed to see her stats to know when she would come out of this terrible ordeal. I remember believing Lucy had a connection and could tell her we loved her and to stay strong and could get through this, even if we had yet to find the cause. The social worker on call came in and asked us if we needed anything. I didn’t have my phone to call anyone to tell them we needed support. I asked the social worker if I could use her phone to call my mother and tell her to get here. She called the rest of my family but we still didn’t know what or why this was happening.
Finally they decided to xray for any diagnostic information they could gather. Seconds after we had the news. Jocelyn had Necrotizing Enterocolitis or NEC. NEC is when the bowel is dying and causing a septic infection. We had known very little about it up to this point but had known that it was something the doctors were always looking out for. Also up to this point she had NO symptoms of NEC. I mean I just snuggled her in my arms hours before all this happened and she was in no way in any distress. The general surgeon rushed in and explained to us what needed to happen in an attempt to save her life. But he made us no promises. He told us he wouldn’t know the extent of the damage of her bowels until he opened her up. He also didn’t know the extent of damage possibly done to her brain of the rest of her organs from being in cardiac arrest. He didn’t know of any outcome but he would do his best to do an emergency bedside surgery to remove the infected tissue. She would need to be on antibiotics to clear the rest of the infection. He would need to leave her abdomen open, intestines in a silo bag to give the rest of the salvageable bowel space to heal. This surgeon also would need to go back in after a few days and remove any more tissue that wasn’t healing. He felt confident in saying this was caused by her heart. That a lack of adequate blood and nutrients to her bowel caused it to begin to die which results in infection. The infection was so bad it put her in cardiac arrest. We consented to surgery, we wanted to give her every chance at life. At this point she had been in and out of cardiac arrest and flat lining for 45 minutes and the outcomes given to us were grave. All we could do was wait in Lucy’s room with my parents and Matt’s family on the phone.
The surgery for lack of better terms was successful. He removed a lot of large intestine. The rest would be up to what her body could heal. This would be an hour by hour day by day situation. Followed by many end of life conversations. But we always held hope that she would pull through and live a wonderful life.
The conclusion to this was as most of you know was miraculous. She ended up having very little small intestine removed and most of her large intestine resected. After the first surgery he left her bowel in pieces and every few hours a nurse had to look into the bag and give a visual report of the status of color and look of infection in the bag. The first 24 hours were tough; it just felt like every time I looked in the changes from black/gray to pink/red were minimal. But after two days she managed to turn for the better and the surgeon came back for the next surgery to re examine. To his pleasant surprise he only removed one more small portion then reconnected her small intestines together and secured them to the surface of her abdomen in the form of an ostomy. He assured us she still had enough bowel left that the ostomy would be temporary and in a few months when she got a bit bigger he would re attach all her intestines and we would go from there.
Next we met with one of the most wonderful women. She was a gastroenterologist that specializes in Intestinal Rehab Patients (IRP) or kids that had surgical NEC. We didn’t know at the time this doctor actually heads the IRP program, but it was clear how smart she was and her talk with us gave me hope even if she didn’t know it. She explained at this age when kids lose bowel they adapt and will actually regrow some intestinal tissue. She was happy to hear how much small intestine she had left. Made her confident she will grow but it will be a challenge at times and that the likelihood NEC would happen again even with her cardiac defect was extremely minimal. This is where the talks became tough from cardiology. They needed her to show she could grow and heal before they would ever consider her surgical heart interventions. Due to the amount of bowel she had left she felt it was very unlikely she would do so. She explained she hoped she would be successful but in her experience has no inkling that it actually will. And rarely she was ever wrong. After about two biweekly meetings with Jocelyn’s care team, cardiology and gastro. Matt just straight up told the cardiologist she was about to be wrong. Looking back makes me giggle because we had no way to know for sure, but at the same time watching her everyday gain a little weight or hit goals they set we knew she was going to be okay. I remember when she first opened her eyes after this whole ordeal, I saw her. I saw my beautiful baby girl was still there and ready to take on this fight. I can’t ever seem to explain how I knew but I knew. Doesn’t mean I wasn’t always freaked out or don’t panic though over the smallest of things. As for her brain, as mentioned before, she’s been fine hitting milestones later than Lucy of course but Jocelyn’s road has been very different, detoured with many surgeries and hospital stays. But for us and every specialist, so long as she is progressing she will eventually catch up.
For those that are curious about that cardiologist, she is truly an amazing and smart woman. She always kept it real with us even if she was certain Jocelyn wasn’t going to come out the otherside the way she has. No she isn’t our regular cardiologist now, but we still email her updates on the girls and she always visits anytime Jocelyn has been inpatient. Now she jokes with us about Matt telling her she was wrong. I will forever be grateful for her.
Where are we today? Well she’s doing GOOD. Growing and gaining weight can be a challenge but she always seems to have a good height to weight ratio according to her gastroenterologist. She has very little large intestine. Most of the large intestines job is to reabsorb water into the body and form poop. Because she has so little we have had to battle some really brutal diaper rashes, even to the point of skin breakdown. She basically used to have constant diarrhea. However now since she eats some solids and purees she no longer has such an issue with diarrhea. Her bowel is adapting and compensating which is fantastic. She has made an amazing recovery and we will be forever thankful for the whole NICU team that saved her life.