After 16 months I am finally ready to publicly share Jocelyn’s heart condition in its entirety. I have put this off for a lot of reasons. One being I didn’t want people if they knew how complex to look at her differently. I never wanted people to set expectations for her physical or mental abilities. What I have learned however is that most people won’t ask me or my husband directly. So like whisper down the lane, I have heard things other family members or friends have said regarding her heart, how it works, or the surgeries she will need. If you know how whisper down the lane works, then you know most of what’s being shared is grossly wrong by the end. Believe me I know why some people don’t ask, maybe they fear my reaction, maybe they think it’s something I’m not willing to share since I never put it on Facebook or any public forum. I guess some of that last part is true, but I felt like I was mostly trying to ward off unsolicited advice or opinions from people who simply just don’t understand. It’s honestly really hard to be this vulnerable though. To be ready to get asked hard questions, some I may not ever really know the answer to. While her heart condition is a very big condition she does also have some other unique things wrong that complicate her much further, but I will discuss those at a later date. Today we are going to let her heart shine!
Here is her official diagnosis’s at birth:
- Hypoplastic Right Heart Syndrome (HRHS)- right ventricle of her heart is small and under developed
- Pulmonary Atresia- no main pulmonary artery segment to carry blood to lungs
- Right Ventricular Aorta- instead of starting at the left ventricle it feeds the body with blood mainly from the right
- Large muscular VSD (hole between both ventricles)
- Bilateral Superior Vena Cava- two superior veins coming from the upper body instead of one
- Discontinuous branch pulmonary arteries coming off aorta
Two more were added after her Glenn open heart surgery :
- Mild to Moderate mitral valve regurgitation- valve between left atrium and left ventricle leaks
- Right ventricle as a whole mildly pumps
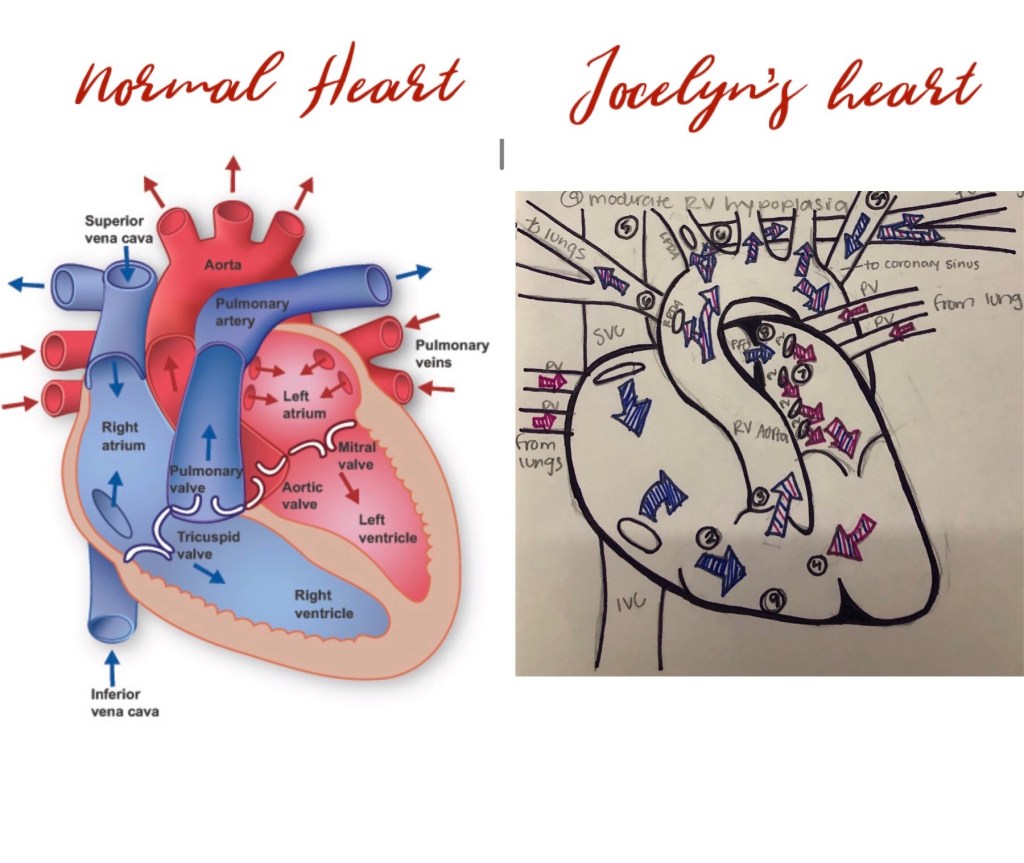
Like I said above she is relatively complex so I’m going to do my best to explain on top of the best pictures I have in demonstration of her heart (mostly because i’m a visual learner).
Let’s start with what a normal heart looks like compared to her heart at birth:
Because she is mainly classified as a Singular Ventricle child our best options were the 3 Step surgical plan. This step by step surgical interventions creates a one way path for blood to get to the oxygen from the lungs and to the body and low oxygenated blood to get back to the lungs. The surgeries goes as follows:
- BT Shunt- For this first surgery they added a shunt off the descending aorta along with using Gortex to connect both pulmonary arteries coming off aorta to provide a pathway to her lung that was as even as possible. This allowed her to come off a medication called prostaglandin that was keeping her able to pass some blood to her lungs to be oxygenated. Normal blood saturation levels for this procedure should be above 75%. Jocelyn sat mostly in the 80-82% range. Most children can receive this surgery about 4 days post birth however in our case Jocelyn didn’t receive hers until about 5 months after birth. We had other complications to overcome first. Unfortunately I don’t have a post BT Shunt drawing however in the post glenn one you can see the connected pulmonary artery they built under her aorta, just looks like a tunnel type of vessel.
- Glenn- This next step surgery they disconnect the superior vena cava (SVC) from her right atrium and connect it to her pulmonary arteries they made for her in the previous surgery. In Jocelyns case she had two SVC’s, therefore both were disconnected and reattached to those arteries, making this a Bilateral Bidirectional Glenn. Normal blood saturation levels for this procedure should be mid to high 80%’s. Jocelyns currently sits around 88%. Most cardiac kids have this second surgery around 5-6 months of age. Jocelyn had her BB Glenn at about 9 months old. In her case we found out she was in heart failure and that we were lucky to be able to get her out so she could have this Glenn procedure done. No she is no longer in heart failure and I will touch more on that story later on.
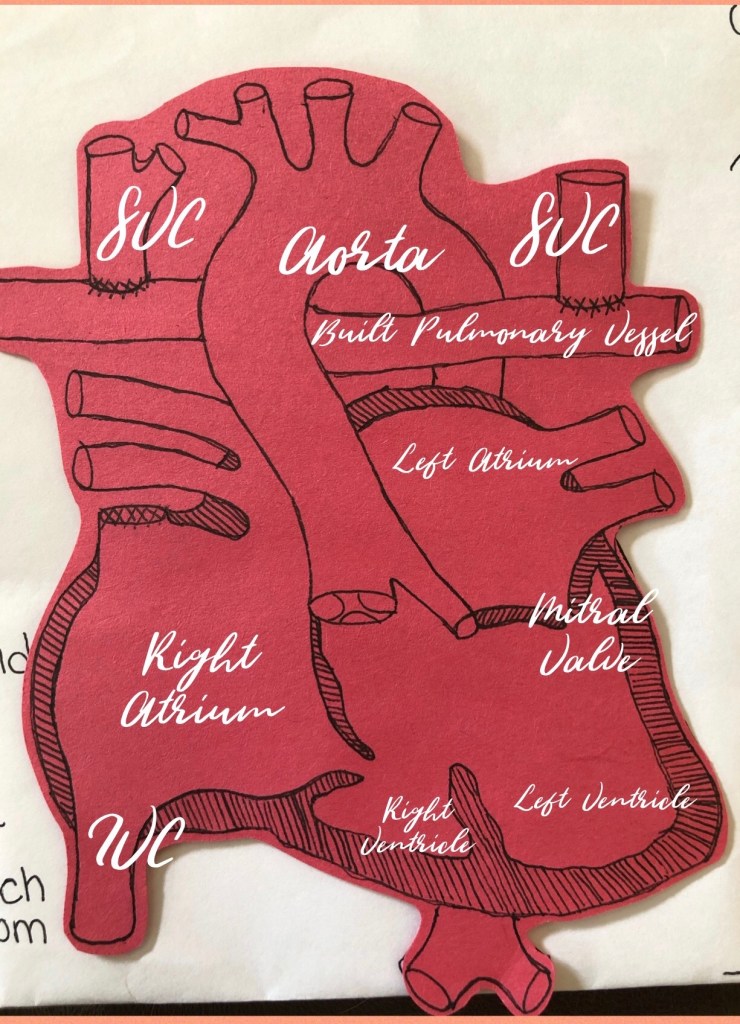
- Fontan- This is hopefully the last open heart surgery. This surgery will require the doctor to disconnect the Inferior Vena Cava (IVC) from the right atrium and reconnect it to the artificial pulmonary artery he previously built. This completes the final stage of the loop. Her blood saturation levels should sit in the low to mid 90%’s. Most cardiac kids will receive this last one as early as 2 years old and as late as 3.5 years old. It really depends if some kids need it sooner. By that I mean their saturation levels slowly start to dip. So no I do not know when jocelyn will have this last surgery but i’m sure she will let us know.
In her case she will also have some lymphatic work like I mentioned in a previous post. If you’re interested in reading that story please feel free to check that out.
I plan on letting her live the most normal life I can provide: soccer, gymnastics, dance- whatever she desires to do. I will implore the same normality when it comes to schooling. I will set no limitations to her success. Lucy is a good support system. She pushes Jocelyn to try her hardest to do the things Lucy can. And for that I’ll always be thankful she has a lifelong best friend and confidant.
Congenital Heart disease (CHD) is a lifelong battle. While the numbers are mainly stacked for our kids it’s still a vicious disease and unfortunately not every child wins the battle. One in a hundred babies are born with a congenital heart defect and more common than childhood cancers. It’s important we raise awareness for funding in research and therapies for these children. Support is important so I always advise every parent with a CHD baby to find theirs.
Jocelyn is a tough cookie and has undergone way more then any child should ever have too. She has never been shy in making her own way through this. So like many parents we follow our child’s lead and pray we are supporting them in every way possible down the right path. I am so immensely proud of her and always in awe of her strength.
Thank you for taking the time to read and learn all this, I know its not easy. I just hope I have done it justice in my explanation. Please reach out with any questions here, facebook or anonymously. Im ready to share no matter how tough.
“Sometimes when i need a miracle
I look into her eyes and realize I have been given so many.”
Forever Jocelyn Strong
